Injury is no fun, but it happens at an alarmingly high rate among musicians. The exact number varies. In an Australian study of orchestral musicians, 84% reported pain or injury that interfered with their playing. In another study, 76% of musicians between ages nine and twenty-four reported that they had experienced pain during playing but only 56% felt like their complaints were taken seriously.
It’s generally accepted by our society that athletes will suffer injury and return to their sport, yet compared to athletes, musicians are even more likely to make a full comeback. In a 2009 study of injured musicians, 97.7% returned full time to playing after undergoing hand surgery. In contrast, only 63% of athletes undergoing ACL repair returned to participate in their pre-injury sport and only 44% returned to a competitive sport.
Regardless of whether the injury is chronic or acute, the body wants to heal and will begin healing as soon as the injured individual takes steps that create space for the natural repair process to unfold . My hope is that the straightforward, actionable tasks in this guide will offer some hope and guidance for managing the conundrum of injury.
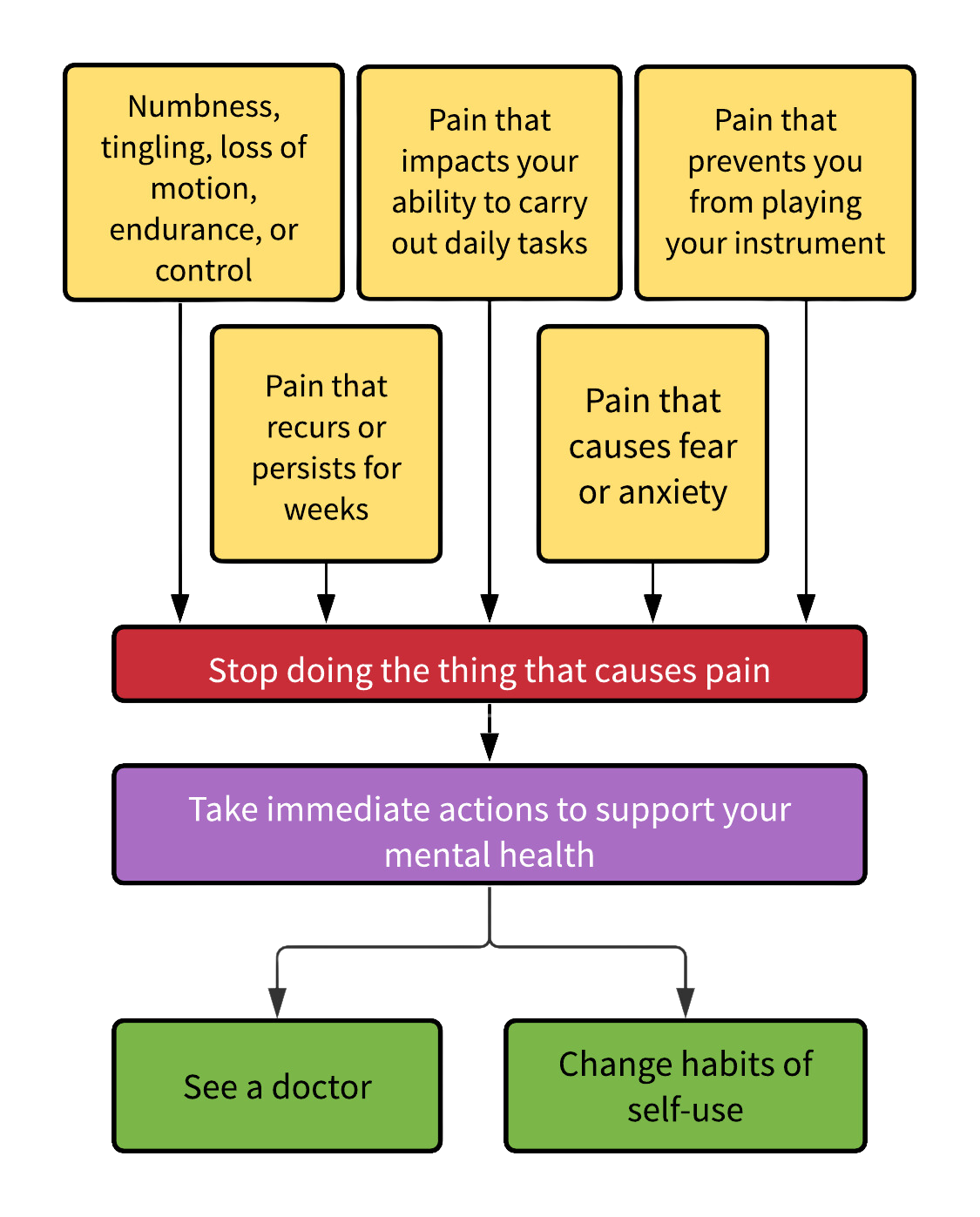
HOW DO YOU KNOW IF YOU ARE INJURED?
Your injury requires medical attention if you experience any of the following:
Sensations of numbness or tingling
Loss of range of motion, endurance, or fine motor control
Pain recurs or persists for more than a few week
Pain that impacts your ability to carry out daily tasks, including playing your instrument
Pain that persists, even during rest
Pain makes you feel anxious or fearful
STOP DOING THE THING THAT HURTS
It’s not worth it to push through the pain as this will make an already bad situation much worse. Notice what causes an increase in pain, such as a particular activity, movement habit, or piece of repertoire. Stop playing your instrument altogether if you have to. The break from your instrument may not necessarily be long, and it’s more likely to be short if you promptly stop playing at the onset of pain. (More on that below…)
If daily tasks are painful, ask someone to help you complete them. Lock your cell phone in a cupboard and forget that it exists for a while. Rest and treat yourself with the utmost care while you seek support from professionals.
TAKE CARE OF YOUR MENTAL HEALTH
Although this might seem like a strange second step, it is essential. By taking early action to support your mental health you will get the most value from your efforts to heal. Injury is likely to impact not only your musical life but also your daily life, and this can be a tough thing to deal with.
The landscape of the mind has a direct impact on physical well-being. Mental stress leads to physical stress, and that stress alone can increase the likelihood of injury. Additionally, research has shown that pain-catastrophizing and fear of pain impact pain sensitivity and intensity. Yes, anxiety can make you physically hurt!
It is worthwhile to foster feelings of safety and well-being because these mental states will actively work to decrease the pain you experience from injury. Set the stage for healing to begin by taking charge of your mental health. You can begin this right away, and it doesn’t even require a doctor's visit.
HOW TO CARE FOR YOUR MENTAL HEALTH
Accept your situation
Talk to someone
Increase self-compassion
Learn about pain and injury
ACCEPTANCE
When we fight against reality it creates additional agitation, anxiety, and stress, and these mental states make it tougher to heal. By compassionately accepting the facts of a situation, we instantly mitigate stress and improve wellness. The acronym “RAIN” created by therapist Tara Brach, provides a simple structure to mindfully manage life’s challenges and it works wonders for the constant frustration of an injury. The steps below may take a bit of practice, but this skill will increase your resilience in the long run.
Recognize what is happening;
Allow the experience to be there, just as it is;
Investigate with interest and care;
Nurture with self-compassion.
Here is an example of RAIN in action:
Recognize: My hand hurts whenever I play this etude and this makes me feel devastated.
Allow: Although I don’t like it, I’ll allow myself to feel the feeling of sadness in my throat and the pain in my hand.
Investigate: As I’ve investigated, I’ve realized that I’m trying too hard to solve the problem on my own. I need to let it go.
Nurture: I know it’s not my fault that my hand hurts and I believe firmly in my capacity to heal. I know that being kind to myself means taking a break and seeking outside support.
TALK TO SOMEONE
Healing is easier when we are supported by friends, teachers, colleagues, and physicians and finding someone to support you as you wade through the emotional repercussions of an injury is essential. Injuries can bring up confusion as well as intense feelings of shame, blame, guilt, and grief. It is natural to feel like hiding your pain or withdrawing from your social circle. Don’t hesitate to seek out professional mental health counseling if you need it. (Or even if you think you don’t!) Some mental health professionals even specialize in helping patients manage pain and illness and preliminary studies have shown that Cognitive Behavioral Therapy is an effective way to improve hand and arm pain specifically. Although there is a mental element to injury and pain, it does not mean that the pain is “all in your head.”
INCREASE SELF-COMPASSION
Researchers are in the very early stages of studying how self-compassion can improve athletic performance and health. Psychologists from Duke University state, “Self-compassion may be a useful way to enhance self-regulation in ways that promote health and adaptive reactions to health problems.” Self-compassion and self-regulation are skills worth building because they ultimately enhance music practice. We engage in safer and more mindful practice when we listen deeply to our needs and attune to the introspective self. Additionally, self-compassion works to soften the blow of an injury that appears to have occurred as a result of our own actions. You can actually measure your current level of self-compassion using this handy test from researcher Kristin Neff. If you determine that your self-compassion could use a boost, Neff’s website is dedicated to the topic and includes highly recommended books on the topic such as Radical Acceptance by Tara Brach and The Gifts of Imperfection by Brene Brown.
LEARN ABOUT PAIN AND INJURY
If learning more about your injury makes you feel hopeful and empowered, then by all means consult Dr. Google. I’m a huge fan of the Pain Science Blog as a resource for the most up to date science about pain and injury. However, wait to be educated by your physician if reading up on your injury causes stress or fear.
Recent advances in the field of pain management have led to the development of an app for managing persistent pain called Curable. This app is intended for pain that usually is referred to as “chronic,” lingering after an acute injury has healed. I practice many of the Curable exercises on a daily basis as I’ve learned some go-to tricks that quickly take the edge off of pain. The app teaches techniques like meditation, reframing, imagery, and journaling to increase self-compassion and improve overall sense of well-being. As I mentioned before, these states also correlate with lower pain sensitivity and intensity. This app is absolutely worth the subscription, especially if your pain is stubborn.
SEE A DOCTOR
Don’t skip this step! Seeking out a medical treatment will grant you the peace of mind that you have done due diligence and provided the best care for yourself. A doctor can provide valuable data and care that no one else can. It is essential to know what type of injury you are dealing with. Going to the doctor is never a first choice as it can be hard on our schedule and budget. However, in the case of an injury that impacts your ability to make music, going to the doctor should be the very first line of action.
WHO TO SEE
Often a general practitioner is the best place to start since they can refer you to the best specialists in their network. If your injury is complicated you might need to see a few different specialists such as a rheumatologist, neurologist, or surgeon. If you don’t like what one doctor tells you, seek out a second or third opinion. If you keep asking questions, eventually you will get the help you need.
I highly recommend working with at least one physician who will take inventory of your complete, overall health. Many injuries and movement disorders are linked to the functioning of the immune system and nervous system. Dystonia is typically treated by neurologists and arthritis is treated by rheumatologists. Frozen shoulder is more common in people with underlying conditions like diabetes and thyroid conditions. I developed a dystonia-like condition in my neck, which resolved when I moved out of a home with a mold problem. Physical therapist, Heather Carr, writes about how her chronic ankle tendonitis resolved after she changed her diet. While some injuries may simply need a bit of R and R, much can be gained from a holistic, multisystem approach to health.
TREATMENT
Treatment typically involves rest, reducing inflammation, and retraining movement habits, usually through physical therapy. (I highly recommend PRI physical therapy if available in your area.) Doctors sometimes suggest alternative therapies such as massage, chiropractic, or acupuncture. Don’t be alarmed if you need to try a few different treatments to get the results you want. Each trial of a new therapy provides additional data about your injury and yourself. You will learn a great deal about your mind and body through the healing process, and this learning will improve your musicianship and performance. Plan to continue a particular therapeutic approach when it gives you good vibes as well as good results. You get to choose who you work with, so actively seek out practitioners that make you feel supported and heard.
REST
Rest is essential, but it is also possible to gently and mindfully return to playing very early on in the healing process. Most physicians want you to get moving as soon as you possibly can. After hand surgery, (which is rarely recommended) the majority of musicians in this retrospective study were able to return to a limited amount of playing in as little as a week and as long as five weeks.
The first doctors I saw actually told me to keep playing but to simply begin practicing gradually and with caution. Yes, I did have to cancel a few gigs in order to accomplish this, but I never completely stopped playing my instrument aside from a day off here or there. The amount of rest you need will be determined by your injury and the input of your doctors and therapists.
The safest way to return to playing is under the supervision of a medical professional who can advise you on the appropriate amount of practice and assist you in adapting your playing to avoid reinjury. The Return to Play Schedule created by physiotherapist Patrice Berque provides a structured framework for safely resuming your playing. Whatever you do, absolutely avoid whatever it was that got you flared up in the first place. Be kind to yourself, ease into playing, and prioritize comfort.
CHANGE HABITS OF SELF-USE
Self-use describes how one uses the entire self to complete a task. While the term technique typically refers to specific movement strategies such as forearm rotation, the term self-use encompasses conscious and unconscious habits of the mind and body, and how these many factors impact the way a person carries out a task.
Changing habits of self-use can be highly empowering and the process often boosts feelings of control, agency, hope and well-being. The insights a person gains from adapting their way of being in music and in life lead to increased happiness, creativity, strength, and resiliency. Injury sucks, but it is an opportunity to change your life and your musicianship for the better!
The specific movements that contribute to injury will vary from person to person, but generally musicians with healthy technique employ a wider variety of movements than those who are injured. Specific habits such as twisting at the wrist can quickly become detrimental. Posture, shoulder mobility, and adequate use of force can also play a role.
It is difficult to accurately perceive our own patterns of movement and even more difficult to unearth new movement options without assistance from another person. Written materials and videos provide facts about body movement, but these facts are not enough to ensure that movement is healthy. Hiring a guide to assist with learning new habits of movement is a requirement!
Below I will cover two of the most frequently recommended approaches for musicians outside of physical therapy (which is also recommended). Combining the study of a specific instrumental technique with a broader, whole body movement practice will produce the best results. Additionally, many of these methods teach mindfulness skills that improve our ability to protect ourselves against future injury. Skills such as self-regulation, awareness, and self-compassion are possibly more important than the movements themselves and will ultimately guide us to find movement that is safe, comfortable, and effective.
TAUBMAN TECHNIQUE AND THE GOLANDSKY INSTITUTE
A Taubman trained teacher guides a student through a structured program intended to completely retrain playing habits for injury recovery and prevention. The teacher will introduce new movement strategies geared towards optimizing alignment, timing, use of momentum, and use of the arm, to name a few. This method moves very slowly at first, but the gradual return to playing makes it safe, and this work typically results in an effortless, pain-free way of playing. This approach is absolutely worth your time and patience.
Now that online lessons are a thing, it’s possible for anyone anywhere to study with a Taubman trained teacher. In addition to written materials, masterclasses and a summer seminar the Golandsky Institute offers a video streaming service so that teachers and students can have constant access to resources that promote healthy movement. This book is an excellent starting point for deepening understanding of essential movements for protecting against injury. This method started with piano as the main focus, but many teachers also work with other instrumentalists.
THE FELDENKRAIS® METHOD
The Feldenkrais Method is a method of movement education that teaches students to optimize movement through an anatomically informed process centered on awareness and ease. Effortless movements are rarely harmful, and learning to prioritize ease is an integral part of the healing process. The Feldenkrais method works with both mind and body and promotes essential skills such as self-regulation and self-compassion. These skills calm the nervous system and enhance the learning process. The emphasis on awareness teaches students to attune deeply to their physical self and this adds an extra layer of protection from injury. The process is safe and not only helps students learn healthy movement habits, but also teaches fundamental skills for optimal learning and practicing.
Students of this method can attend group Awareness Through Movement® classes or work one-on-one with a practitioner in Functional Integration® sessions. There are many online resources, including free class recordings. This blog is dedicated to this method, so you will also find information here. Click here for a directory of Feldenkrais Practitioners who specifically work with musicians.
OTHER MODALITIES
I’ve focused on the modalities above because I know that they have been highly effective for many, many people. Other bodywork methods include Anat Baniel, Alexander Technique, Aston-Patterning, Franklin Method and Pilates.
MOVEMENT INQUIRIES
Movement practitioners that help students form new playing habits may inquire about various aspects of your self-use. These are just a few questions they may ask.
How do you sit?
What is your typical mental and emotional state during practice? (Ex. mindful, patient, impatient, stressed out, doubtful)
What is the relationship between shoulder and arm? How do you align the hand with the arm?
How much sensation do you feel in your body when you play?
How free are your movements?
How much variety of movement do you employ?
How much force is used to produce tone?
How do you breathe?
Is muscular effort evenly distributed throughout the body?
Even prior to stepping into the office of a specialist you can begin exploring these inquiries on your own.
WORKING WITHIN A BUDGET
The fact is that many musicians are operating on a limited budget and healthcare can quickly add up. Some physical therapists are trained in movement practices such as Alexander or Feldenkrais and sometimes these professionals will bill your insurance. Additionally, many movement practitioners understand that an injured person might be struggling financially and thus offer sliding scale fees to their clients. Additionally, many massage practitioners bill insurance. Look for massage practitioners that are trained in work such as Cranio-Sacral Therapy, Neuromuscular Massage, or Manual Therapy. Acupuncture is often covered by insurance or is available in affordable group sessions, and many people find acupuncture to be extremely beneficial.
Regardless of the price tag, it is absolutely necessary and worth it to spend money on your recovery and health. If you have a family member that is willing and able to assist with the costs then take advantage of their generosity. Although it might be uncomfortable to ask for financial assistance, you will be better off in the long run. I regret not asking my parents to pay for my physical therapy when I first developed an injury. I waited six years to start PT because it wasn’t covered by my high-deductible plan. I would have been much better off with early intervention.
CONCLUSION
Just by reading this you have taken an important step towards healing your injury. There will be lots of decisions and ups and downs ahead. Whatever you do, don’t despair! Injury is temporary. Follow the path that best suits your medical needs as well as your interests and personality. Rest assured that once you take action you will heal and continue to share your music with the world!
REFERENCES
Ackermann B, Driscoll T, Kenny DT. Musculoskeletal pain and injury in professional orchestral musicians in Australia. Med Probl Perform Art. 2012 Dec;27(4):181-7. PMID: 23247873.
Gembris H, Menze J, Heye A, Bullerjahn C. High-Performing Young Musicians' Playing-Related Pain. Results of a Large-Scale Study. Front Psychol. 2020 Dec 16;11:564736. doi: 10.3389/fpsyg.2020.564736. PMID: 33391080; PMCID: PMC7772153.
Butler K, Winspur I. Retrospective case review of time taken for 130 professional musicians to fully return to playing their instruments following hand surgery. Hand Therapy. 2009;14(3):69-74. doi:10.1258/ht.2009.009019
Meredith L. Terry & Mark R. Leary (2011) Self-compassion, self-regulation, and health, Self and Identity,10:3, 352-362, DOI: 10.1080/15298868.2011.558404
Webster KE, Feller JA. A research update on the state of play for return to sport after anterior cruciate ligament reconstruction. J Orthop Traumatol. 2019 Jan 28;20(1):10. doi: 10.1186/s10195-018-0516-9. PMID: 30689073; PMCID: PMC6890902.
Li H, Moreland JJ, Peek-Asa C, Yang J. Preseason Anxiety and Depressive Symptoms and Prospective Injury Risk in Collegiate Athletes. Am J Sports Med. 2017 Jul;45(9):2148-2155. doi: 10.1177/0363546517702847. Epub 2017 Apr 25. PMID: 28441037.
Quartana PJ, Campbell CM, Edwards RR. Pain catastrophizing: a critical review. Expert Rev Neurother. 2009 May;9(5):745-58. doi: 10.1586/ern.09.34. PMID: 19402782; PMCID: PMC2696024.